Foto: Melissa Niemann
Anna Uppströmer sits with her knees drawn up on the examination bed in the oncology department at Skellefteå hospital. In other words, in the ward for cancer patients.
– I haven't collapsed yet. My friends don't understand how I manage, they say I must be incredibly strong. I don't know, maybe I am. But I have no other choice.

Except for her shaved head, it's hard to tell she's sick. Terminally ill. Instead, a smile on her lips and sparkling eyes reveal a strong zest for life. And without it, she wouldn't be sitting here today.
To understand Anna's story, we need to rewind the tape. Six years ago, she was living a normal life in Bureå with her husband and three children. She works as a nurse in a nursing home. But then comes the day that will turn her whole life upside down.

Anna's entire life was turned upside down when she received the cancer diagnosis.
Then 48-year-old Anna underwent a routine gynecological check-up. During the exam, the doctor discovered an irregularity and, out of caution, scheduled Anna for an ultrasound a month later.
– At the time, I wasn't overly concerned, Anna recalls.
– It was just a precautionary measure, an ultrasound. However, during that month, I started experiencing stomach pain and a constant urge to urinate.
Anna waited for the follow-up appointment, hoping it was nothing serious.
– The subsequent ultrasound revealed that my uterus had enlarged to the size it would be at twelve weeks of pregnancy, Anna explains.
– A large mass was also visible on my ovary. The gynecologist downplayed the possibility of a tumor, but things escalated quickly.
A few days later, on a Friday, a nurse from the women's clinic contacted Anna, informing her of a scheduled appointment the following Monday.
–She also requested that I bring someone with me. That's when I knew that this wasn't just a simple matter.

Much time has been spent inside the oncology ward at Skellefteå Hospital
Following a nervous weekend, Anna and her husband, Niklas, braced themselves in the waiting room at the women's clinic. Then came the dreaded diagnosis: Anna had advanced ovarian cancer with metastasis. Surgery to remove the tumor was deemed necessary – immediately. The surgery was followed by chemotherapy, a medication designed to inhibit cell growth and prevent further spread.
– It was like tunnel vision, Anna remembers, her voice heavy with emotion.
– All I could see was an impenetrable darkness. Then, a flicker of light – my children. The overwhelming fear washed over me. I wouldn't get to see them grow up, witness them start families, travel the world... anything. I shut down after that, unable to absorb anything else the doctor said.
Even now, years later as she lies on the bed, chemotherapy coursing through her veins, tears well up in Anna's eyes at this particular memory. It's the heaviest burden she carries – the agonizing fear of missing out on her children's lives.
With a trembling hand, she wipes away the tears, offering a soft apology. Tears aren't her usual response. Surrounded by tubes, needles, and IV drips, a constant reminder of her current state – palliative care, focused on comfort and quality of life in her final stages. Reality can be overwhelming at times, but Anna persists in telling her story.
– Back home, the full weight of it all came crashing down. The doctor's words finally sank in. I vividly remember my mother's embrace... a comforting hug that transported me back to a time of childhood innocence.

Anna believes the oncology ward isn't particularly large, but finds comfort in seeing the same nurses each time she arrives.
The pace of events accelerated dramatically. The family vacation to Mallorca was abruptly cancelled. Anna's surgery, originally scheduled three weeks out, was moved to just a few days away. The urgency of her case necessitated a swift rescheduling by the doctors.
While the doctors were optimistic about removing all the cancer, they cautioned Anna about the potential need for a stoma.
– It wasn't a big deal for me, Honestly, I didn't care if I had to get a stoma as long as they got rid of the cancer.

Chemotherapy treatment.
In Umeå, Anna was prepped and wheeled into the operating room for a critical surgery that lasted for nine long hours.
– Regaining consciousness, my first instinct was to reach down to see if I had a stoma bag, Anna recounts.
– Finding it filled me with an unexpected sense of relief. It was a tangible sign – proof that the surgery wasn't merely exploratory. They had taken action.

Anna believes in a higher power that offers comfort and guidance.
– Before the surgery many of my Christian friends prayed for me and the medical team. So, I felt compelled to tell the surgeon about it.
Her honesty receives a simple nod of acknowledgement. However, after the surgery, the same surgeon pays her another visit.
– He came in and said, 'You know, Anna, I'm glad you told us that many people were praying for us today, because we truly needed it, Anna recounts.
– In that moment, it felt incredibly special, almost magical.

Anna has chronic cancer. That's what it's called when it returns," she explains.
A few days later, Anna is able to return home. Around the same time, she receives a text message from her husband, Niklas, with a picture of a puppy.
– He asked if I wanted her, and of course I did! It was clear that she would be called 'Vinna'. She would be a part of my rehabilitation, Anna says, her face lighting up.
– Vinna has meant a lot to me. Not only does she provide companionship when I go out, but she also gives me something to take care of, she adds.

The dog Vinna has been a big part of Anna's rehabilitation.
A month after the surgery, it's time to start chemotherapy. Throughout the autumn the treatment goes well enough for Anna to partially return to work.
– Every three months, I have a follow-up to make sure everything looks good. But the successes didn't last long, says Anna.
– By May 2020, the cancer had returned, and this time it had spread to my liver. When it comes back like this, it's considered chronic. There's no cure for ovarian cancer today.
Despite her setbacks, Anna remains resilient.
– I've kept my spirits up even when it's been hard. I've never just laid down and given up. I always thought, 'Well, let's get back to it. Of course there have been tears and sad days, but they're often short. When I cry, I pick myself up pretty quickly. I tell myself, 'It's okay, Anna.'
After the cancer returns, it's back to chemotherapy. In February 2021, a new option becomes available, and Anna tries Lynparza, a type of chemotherapy in pill form. It allows her to work part-time for almost a year. She takes the drug until the fall of 2023, when she gets sick again.
– I got very sick with the liver metastases last autumn and had to stop taking Lynparza. But this drug gave me extra time. Now it's just different chemotherapy treatments for me. Every time you get sick, your treatment options shrink. You can't use the same chemotherapy again and again.
She falls silent and stares into space. There's a faint hum of medical equipment in the treatment room of the oncologist's office.
– My life won't be as long as many people's. I don't know what will happen tomorrow or how many days I have left. It's not a good feeling. But you have to try not to dwell on it and learn to live in the here and now.
Outside the fourth-floor window, large snowflakes are falling to the ground. Anna is served a bowl of soup for lunch and fruit soup for dessert. She can only eat liquid food now. The department counselor comes in and compliments her, saying she looks nice with her head shaved. Anna laughs and says she's decided never to let her hair grow again. It feels good to have it short.
It's all hustle and bustle in the chemotherapy ward at Skellefteå hospital. Nurse Ulrika Bergqvist is in charge of the department.
– We treat people who have had surgery, cancer patients, and units from the women's clinic, she explains.
The department is called oncology, or "the chemo ward" among patients. Oncologists are the cancer specialists.
– We are open during the day. Patients who are too sick to be at home are usually too sick to receive chemotherapy, Ulrika adds.

Nurse Ulrika Bergqvist at the oncology ward of Skellefteå Hospital.
– We have a lot of patients, and the number is growing, she says.
What is it like to work here?
I love my job. You get to help people. It's a varied job, and we treat so many different people. The patients are very appreciative. But there are also difficult moments because you can't help everyone. But we can help a lot of people, prolong their lives, and make them fa little better, says Ulrika.

"Despite working with seriously ill people, the job provides moments of laughter," says Ulrika Bergqvist.
Anna's stubbornness, a trait that would prove crucial, came to the forefront in the fall of 2023. Her health took a sharp turn for the worse.
– I started feeling awful back in the summer, but things just dragged on because it was vacation time. I even remember giving a real piece of my mind to a surgeon over the phone for not getting my scan results back.
This decline in health led to another hospitalization. Tests revealed a serious problem – her liver was failing rapidly.
– The doctors basically told me I didn't have long left and there weren't many good options. One possibility was surgery in Umeå, but the doctor strongly advised against it.
But Anna was determined.
– The doctor questioned whether I was strong enough for the procedure. I just told them I had to try. They were worried my body wouldn't handle it and suggested I spend what little time I had left with my family. But my whole family was behind going to Umeå.
After a lot of discussion and to-and-fro, Anna made the trip to Umeå.
– It was a simple decision for me. Staying here meant certain death. Even if the surgery in Umeå wasn't a success, at least I wouldn't have given up without a fight. Maybe I could even squeeze out some more time.
Thankfully, despite the doctor's initial reservations, the surgery was successful. That's the reason Anna is still alive today.
Back home in Bureå, Anna has adjusted to a new normal thanks to palliative care, allowing her to remain at home.
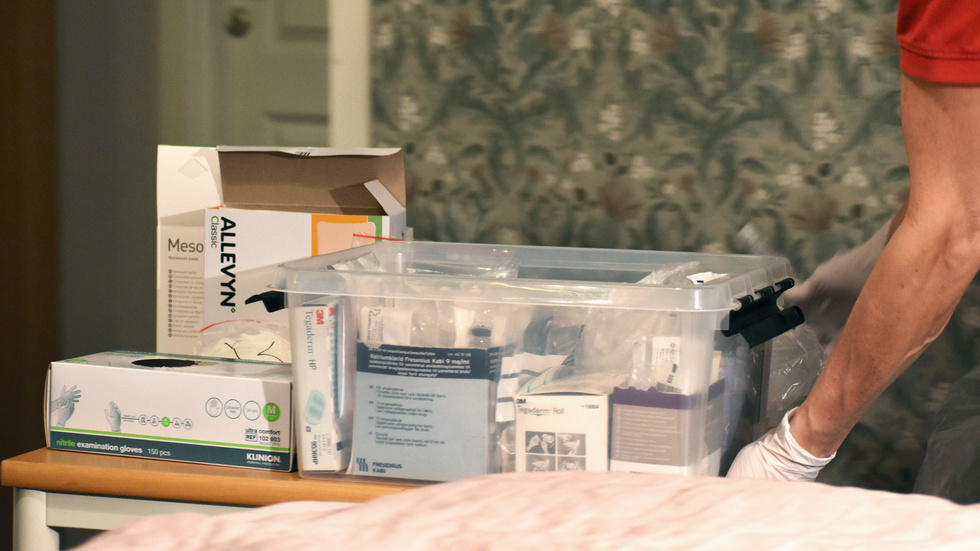
Being cared for at home.
– It's such a relief, Anna says.
– Now I don't have to shoulder this burden alone. Having the palliative care team at home is fantastic. They're not intrusive, but they're there to lend a hand when I need it. I can still be independent and do things I might not have been able to manage otherwise. Palliative care doesn't mean the end, you know.
Despite this newfound support, Anna can't deny the frustration of her limitations.
– It gets to me, there's always something new cropping up, she admits.
– It feels like there's a constant worry nagging at me. But the key is not what happens, it's how you handle it. I have to keep a positive spirit to push through the rough times. There's still plenty of joy to be found in life, even like this.
Every evening, a member of the palliative care team swings by to connect Anna's nutritional drip. She receives nightly infusions through a tube in her arm. Today, it's Nurse Helena Hällgren who makes the visit.

Helena Hällgren from the palliative care team often visits Anna in the evenings.
Palliative care is second nature to Helena – she's been in the field for 25 years. Working closely with end-of-life situations holds a deep meaning for her.
– It's not something that fazes me any more, Helena explains.
– In fact, I see it as a much better alternative to the hospital environment.
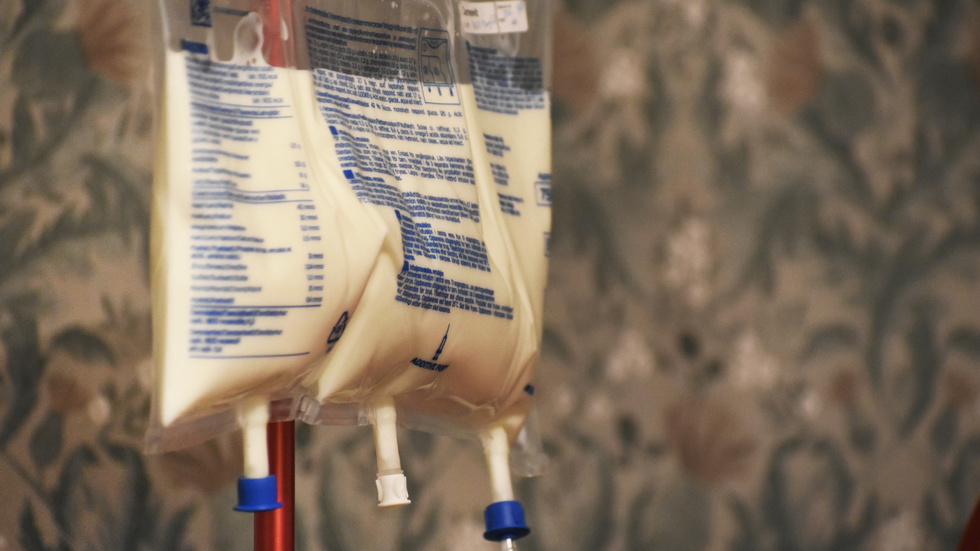
Varje natt får Anna näringsdropp.
In December, Anna found herself back in the hospital. A double whammy hit her – covid-19 and sepsis.
– I felt alright, honestly, but then the doctor called with blood test results showing sepsis. The thing is, chemo messes with your immune system. Normally, sepsis would knock you flat, but I didn't feel that bad.
Treated with intravenous antibiotics three times a day just before Christmas, Anna feared the worst.
– I started tearing up at the thought of spending Christmas stuck in the hospital. Luckily, we found a strong antibiotic that only needed once-daily doses, and the palliative team could even administer it at home. So, I got to celebrate Christmas with my family after all.
The plan moving forward is to continue chemotherapy with breaks every four weeks. But the future remains unclear.
– Eventually, my body won't tolerate the treatment anymore. Chemo wipes out your immune system completely.
The latest scan results are positive – the metastases haven't grown. However, the sepsis forced a pause in chemotherapy, and Anna anxiously awaits news on how she responded during this break.
– The weeks leading up to doctor's appointments are pure torture. I start imagining all sorts of symptoms – more pain, swelling, something's definitely wrong. I turn into a bit of a hypochondriac. Maybe it's a way to brace myself in case the doctor delivers bad news. At least I'll be mentally prepared.
While other treatment options exist, a cure is no longer a realistic possibility.
– This has been a long road. I've accepted that I will die. Don't get me wrong, I don't want to die. But deep down, I know I have to face the reality that it's going to happen. It's not a choice.
– What kind of emotions does that bring up?
– Not good ones. All I want is to be with my family.
Tears well up in Anna's eyes and spill down her cheeks.
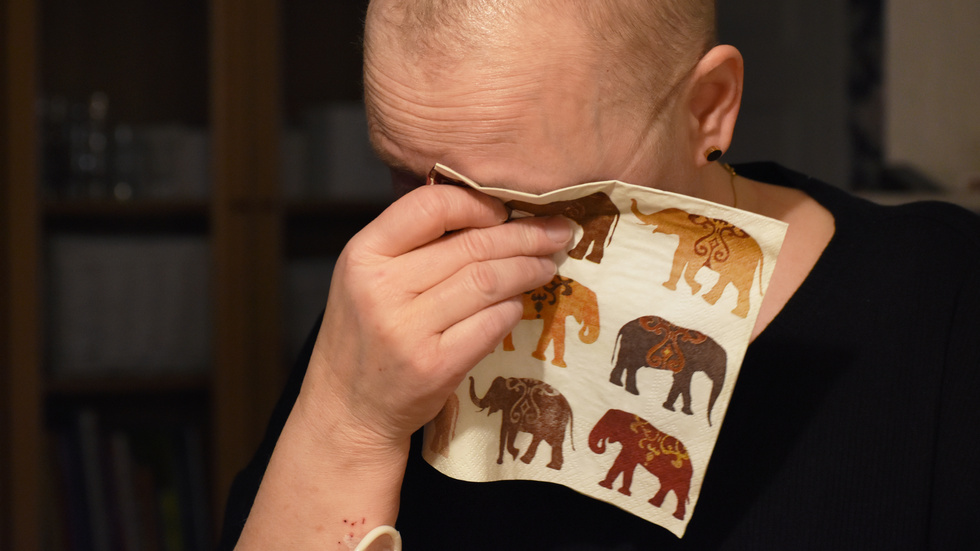
Leaving her family behind is one of Anna's greatest fears.
– There are moments when I wonder how much longer I can keep this up, Anna says.
– How many times can I pick myself up again? But so far, I've managed to do it, so I guess I've got a stubborn streak in me. I can't just lie down and give up.
– I don't know how I'll feel when my final days arrive," she continues.
– For now, I find solace in my faith, and I hope that will be enough then too. With time, I've somehow come to terms with the inevitable, and I can find a sense of peace within it, even though I don't want it to happen. I want to live.



